Team Lecture: Orthodontic-Orthognathic Surgery
By Dr. Karen Piamonte – Miranda
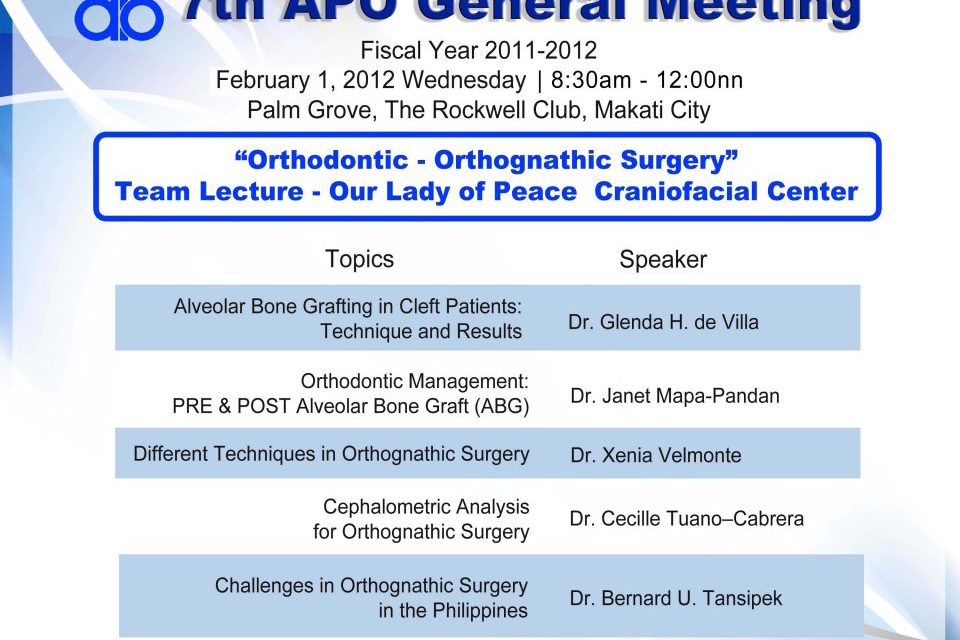
The 7th APO General Meeting held at Palm Grove, The Rockwell Club in Makati City last February 1, 2012 was the first meeting for the year 2012. The venue was packed with APO members and there was a big group of students from CEU in attendance. Everyone was enthusiastic to hear the lecture of the team from Our Lady Of Peace Craniofacial Center, comprised of oral and maxillofacial surgeons Drs. Glenda de Villa and Xenia Velmonte, plastic reconstructive surgeon Dr. Bernard Tansipek and our very own APO members Drs. Janet Pandan and Cecile Tuano- Cabrera. Through their lecture we see the importance of working as a team to address the problem of patients with cleft of the lips, palate and those with facial deformities.
As we have learned, the treatment of patients with cleft lip and palate starts from infancy and continues on to adulthood. After the initial lip and palate repair, there is still an alveolar cleft of the maxillary arch that needs to be closed. Alveolar bone grafting (ABG), using cancellous bone harvested from a donor site in the same patient, is done to closed this defect in the alveolus. ABG completes the maxillary arch, closes the oro-nasal fistula, provides bone for the tooth erupting into the cleft gap, and improves the skeletal support of the floor of the nose. It also facilitates oral hygiene and removes speech defects secondary to the alveolar cleft. Sources of this cancellous bone for grafting include iliac (most popularly used), tibia, rib, calvarium, and mandibular symphysis. ABG is usually done during the late mixed dentition (9-11 years old), the canine is ½ to 2/3 developed, crown is covered with bone.
In cases where orthodontic treatment is done prior to ABG, the goal is to improve esthetics, establish functional occlusion, eliminate or lessen traumatic occlusion, and to establish better access on the cleft site during surgery. After ABG, orthodontic treatment is continued and movement can be started as early as 8 weeks. Cases have also been reported wherein the canines spontaneously erupted in the graft site.
Cases where orthognathic surgery (OGS) is indicated were also presented. Orthognathic surgery is surgery to correct conditions of the jaw and face related to structure, growth, sleep apnea, TMJ disorders, malocclusion owing to skeletal disharmonies or other orthodontic problems. It is indicated if there are anteroposterior, vertical, and transverse discrepancies, asymmetries, and dysfunctions. Different cephalometric analyses were also discussed to determine the degree of these discrepancies. Some surgical techniques that were discussed to correct mandibular discrepancy were sub-apical osteotomy, vertical subcondylar or ramus osteotomy, segmental osteotomy, and sagittal split osteotomy.
The Standard Protocol for OGS is the one we, as orthodontists, are familiar with. The focus of this protocol is more on facilitating the establishment of the correct occlusion during surgery. Thus presurgical orthodontics plays a major role. Alignment and levelling during this stage include reducing or eliminating dental compensation, establishing the desired postsurgical position of the incisors, expand constricted areas in the tapered arch. During the surgical planning stage, several radiographs may be required such as lateral cephalometric film, panoramic, periapical (for segmental osteotomy), posteroanterior (for asymmetry). Cephalometric analysis, paper surgery, and model surgery are used in planning the surgical procedure. After the surgery, orthodontic treatment is continued for several months to finish the case.
There is however a Surgery First Protocol for OGS that was introduced. With this protocol the total treatment time is cut in half since the focus is on establishing good facial esthetics first and a malocclusion that is more “workable” for the orthodontist. The bulk of orthodontic treatment is done after the surgery and finishing the case is much easier since the jaws are already in a more harmonious relationship.